With the growing prevalence of demyelinating disorders, Magnetic Resonance Imaging (MRI) has become the dominant neuroimaging technique for multiple sclerosis (MS), playing a crucial role in diagnosis, treatment monitoring, and disease progression prediction. Conventional MRI techniques, including T2-weighted, T1-weighted, and FLAIR imaging, are used to assess lesions and atrophy in the central nervous system. Advanced techniques such as MR Spectroscopy, Magnetization Transfer Imaging, and Diffusion Tensor Imaging have enhanced our understanding of MS pathogenesis. Complementary imaging technologies like positron emission tomography and optical coherence tomography have further expanded our knowledge of MS. While MRI has provided insights into inflammation and axonal loss mechanisms, the relationship between short-term MRI activity and long-term disability remains uncertain, necessitating clinical endpoints in definitive trials.
In our 20 years of experience in the field of neuroradiology, we have built a substantial archive of confirmed cases of demyelinating disorders. One of the outcomes of this work is a book on Magnetization Transfer Ratio (MTR) and its role in the diagnosis of demyelinating disorders. Additionally, several differential diagnoses have been compiled. Here, we present some of these cases. This extensive archive could serve as a valuable resource for AI researchers and other scientists aiming to expand knowledge about this chronic, devastating disease.
Case No 1
A 40-year-old woman presented with sudden blurred vision.
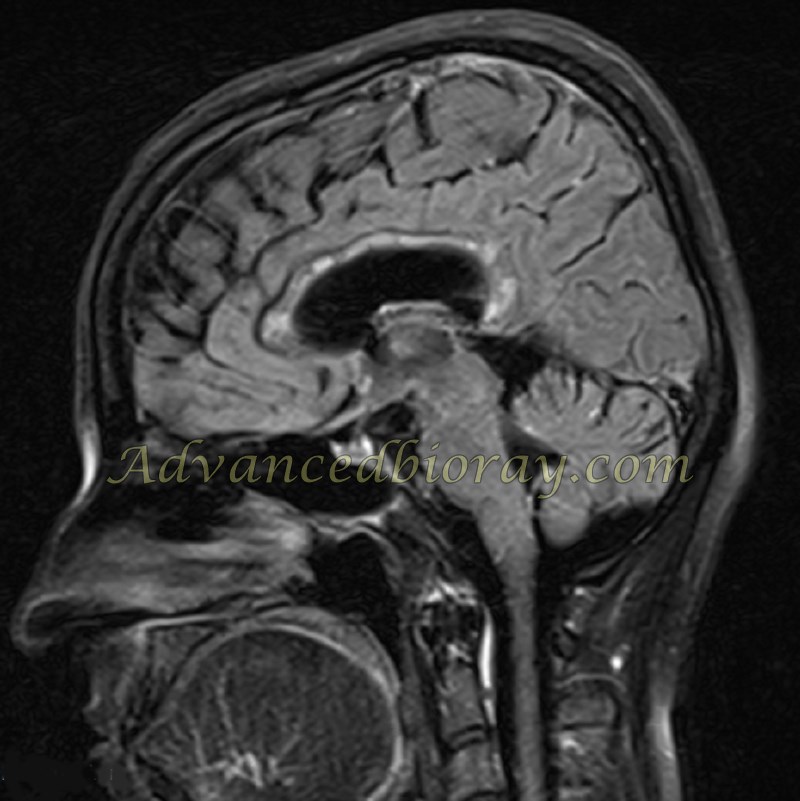
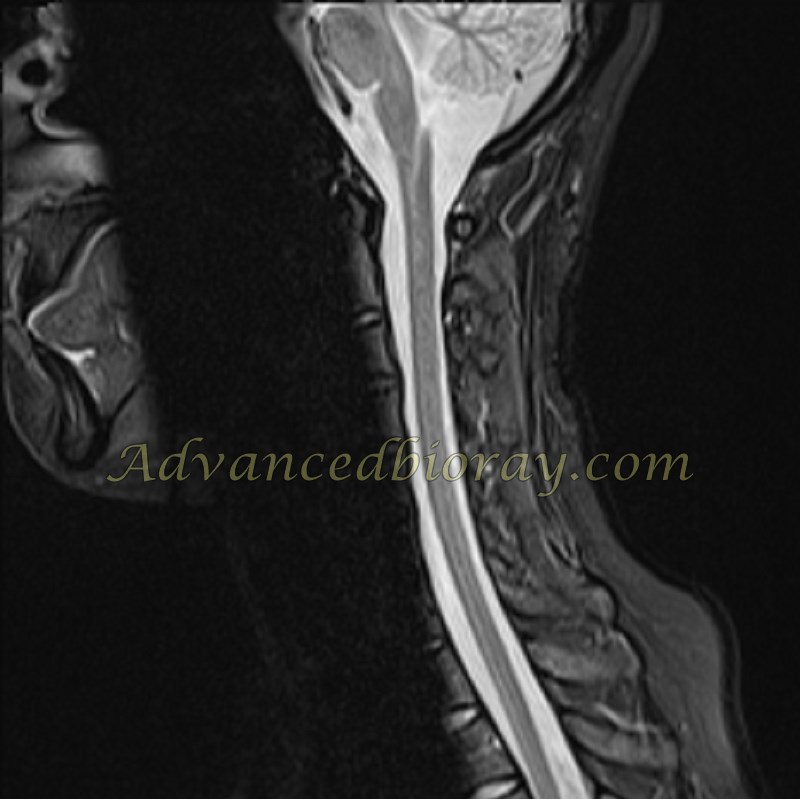
MRI in the sagittal FLAIR sequence shows abnormal pericallosal and periventricular hyperintensities without enhanced plaques on delayed post-contrast MRI. Additionally, the sagittal STIR sequence reveals involvement of the entire spinal cord.
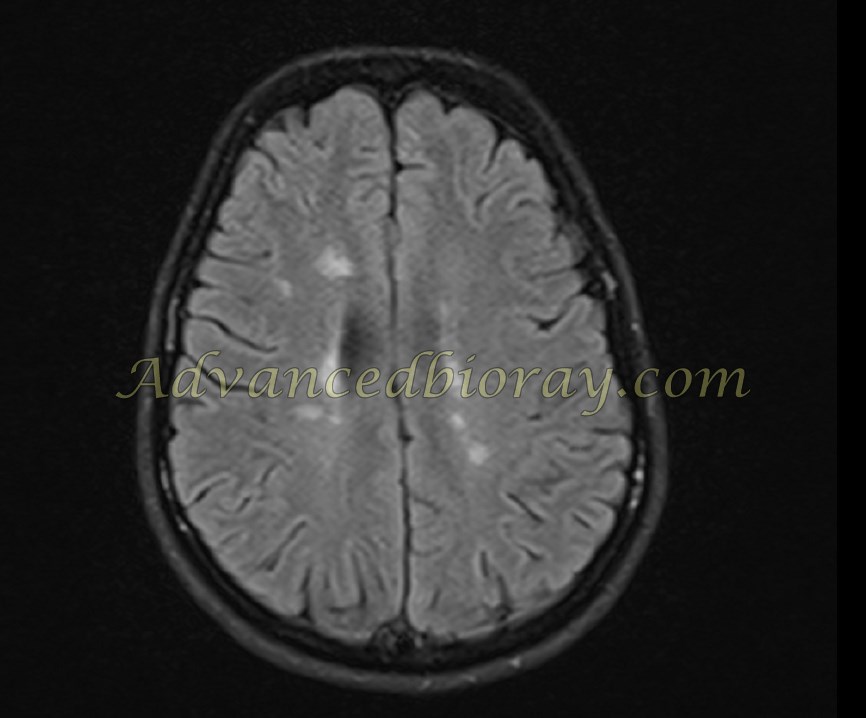
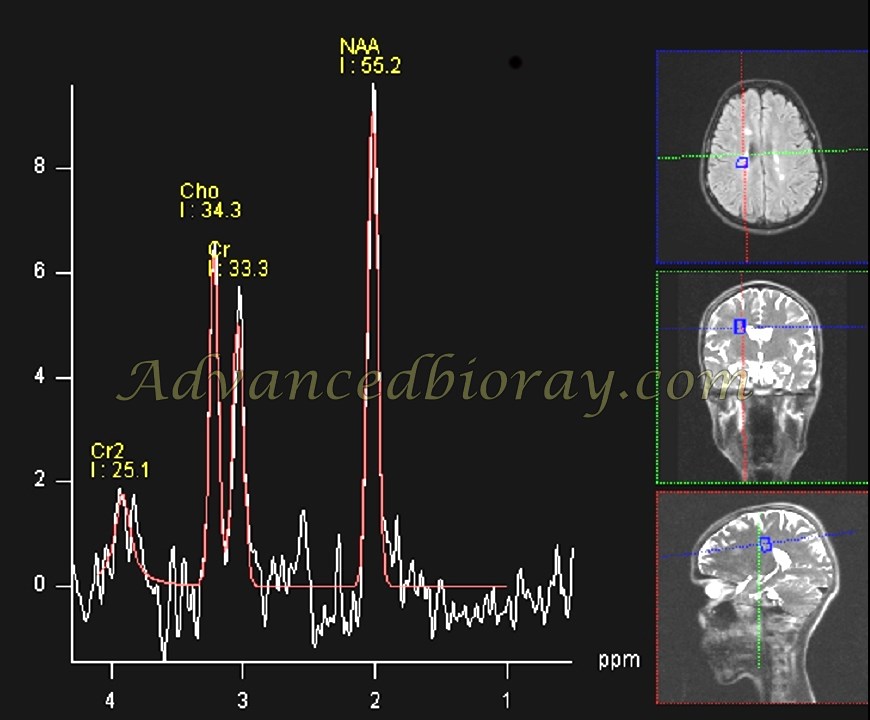
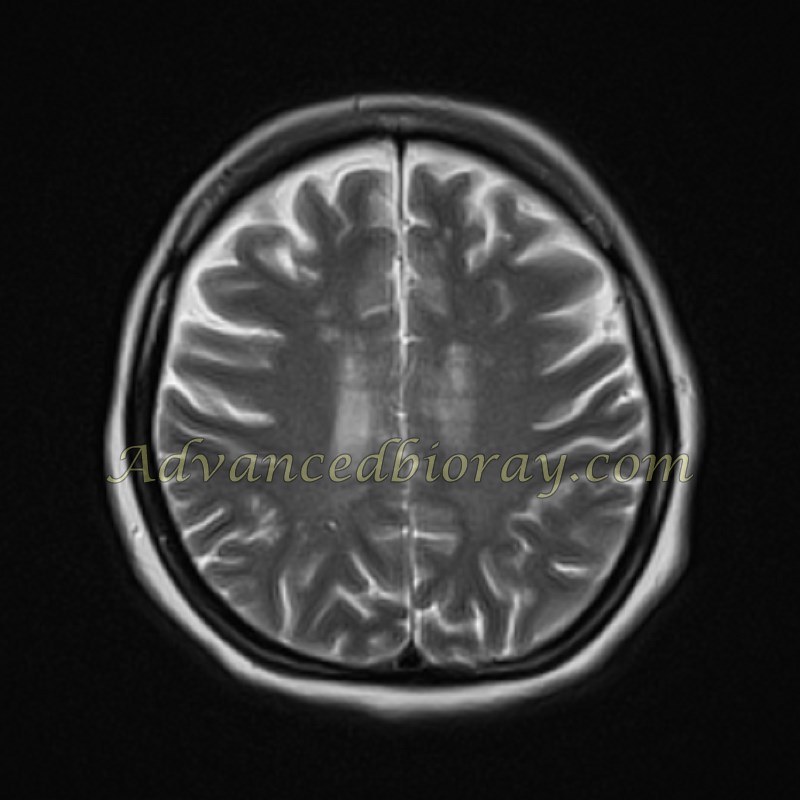
Case No 2
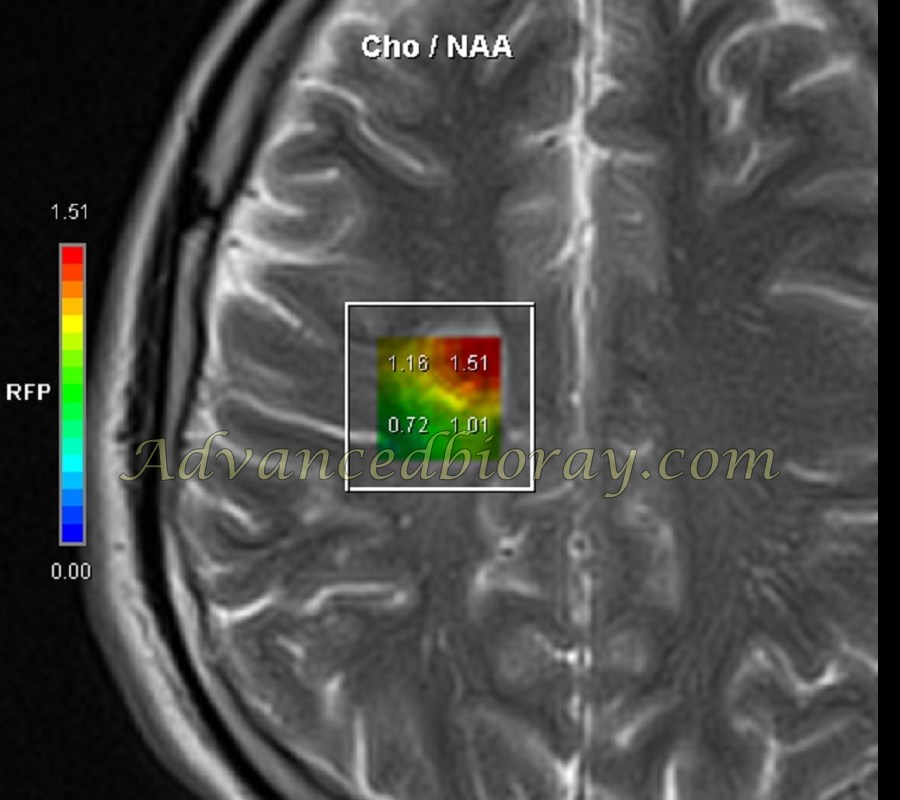
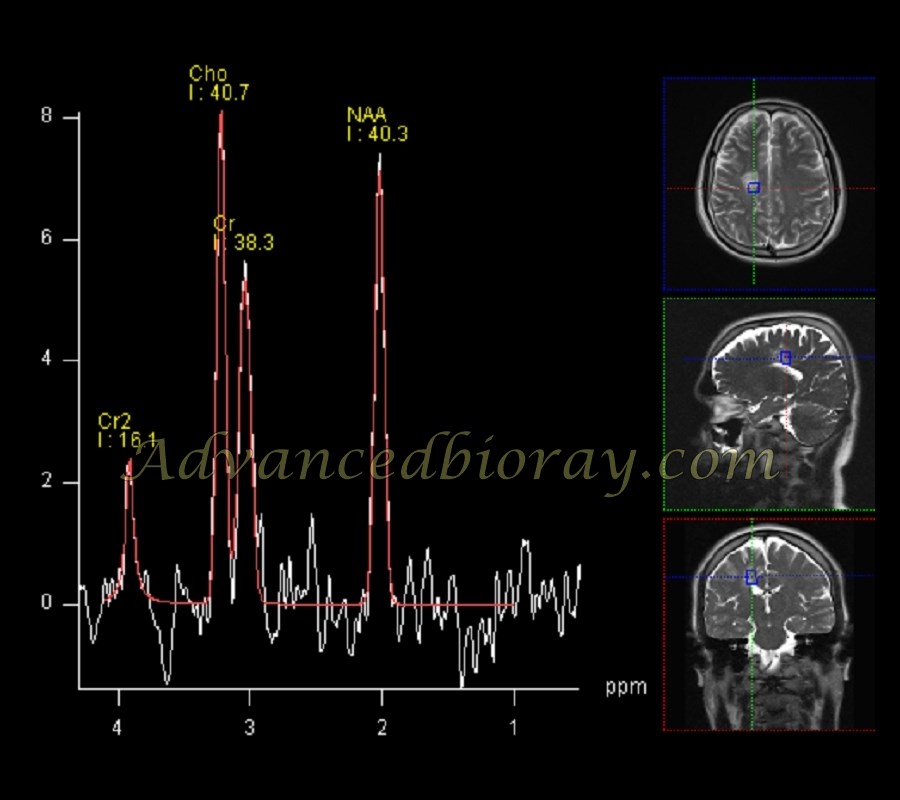
A 39-year-old woman with a history of paresthesia. MRI reveals typical periventricular and pericallosal hyperintensities. MRS in this case shows no typical Cho/NAA ratio increase or spectral abnormality, consistent with the lack of enhancement and no detectable active plaque.
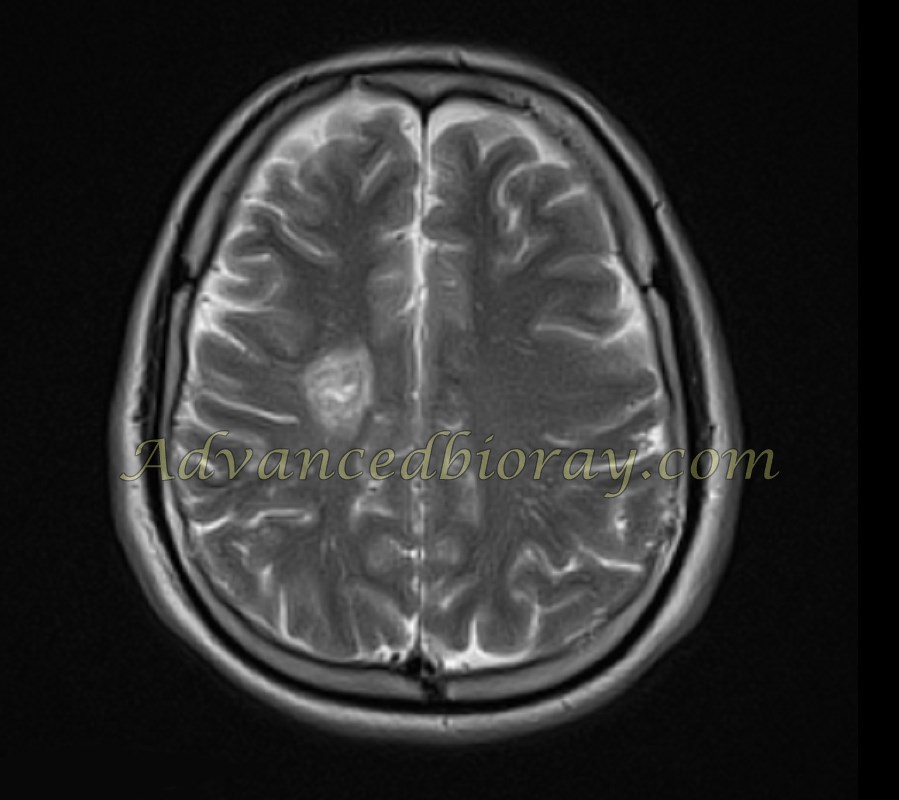
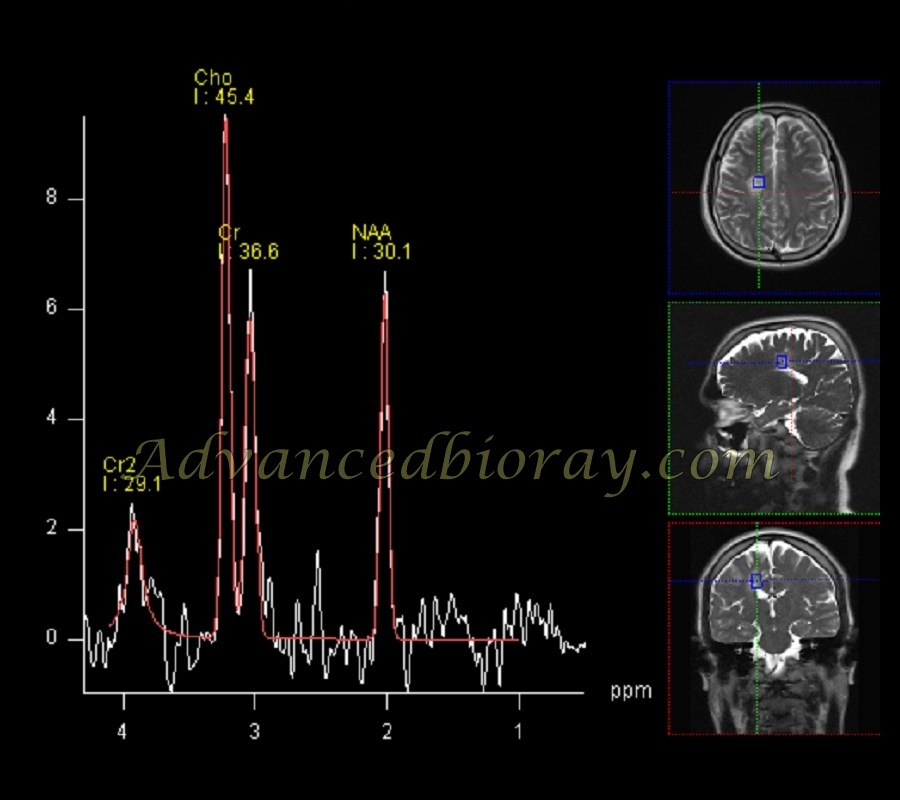
Case No 3
A 22-year-old man with a demyelinating disease. MRS from one of the activated tumefactive plaques shows a Cho/NAA ratio increase, suggesting an acute inflammatory process and an activated plaque. There is also a lactate increase. Clinical findings corroborated the presence of an activated plaque, aligning with the patient’s symptoms.
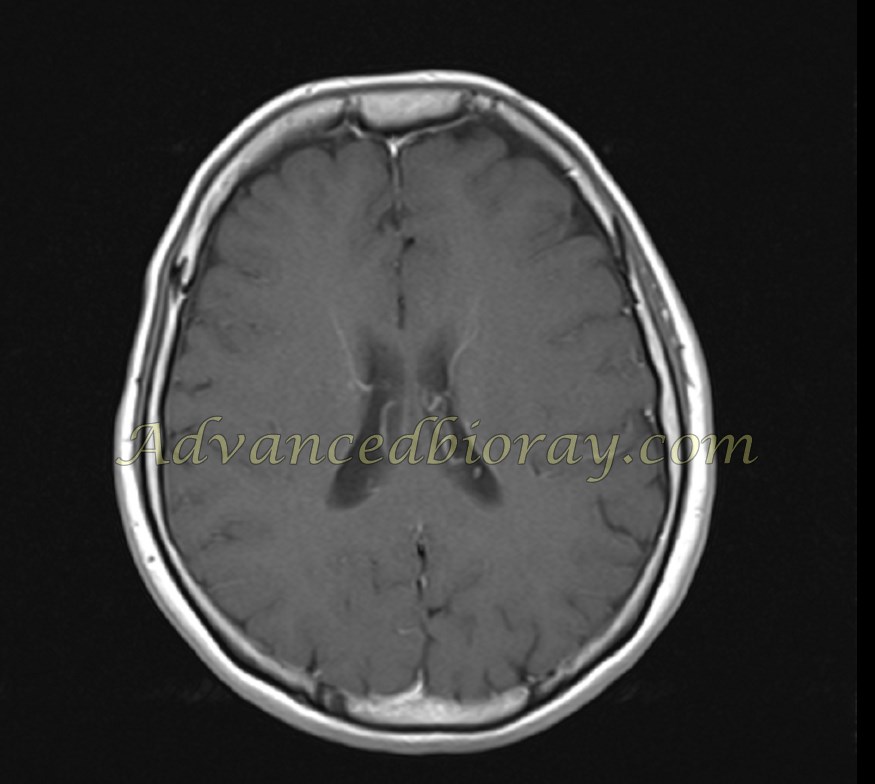
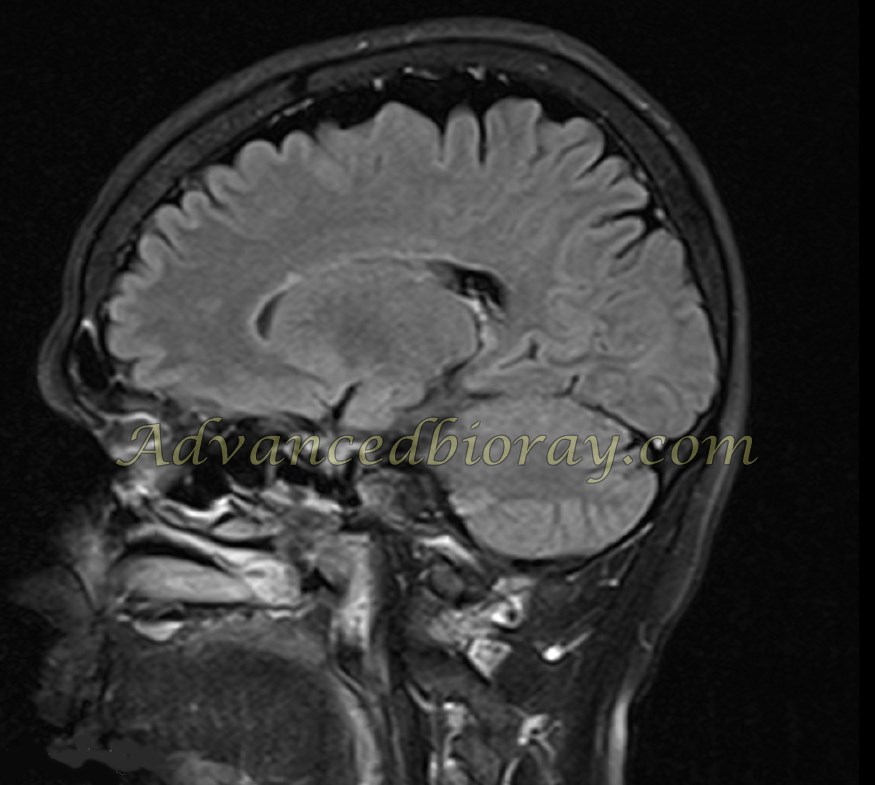
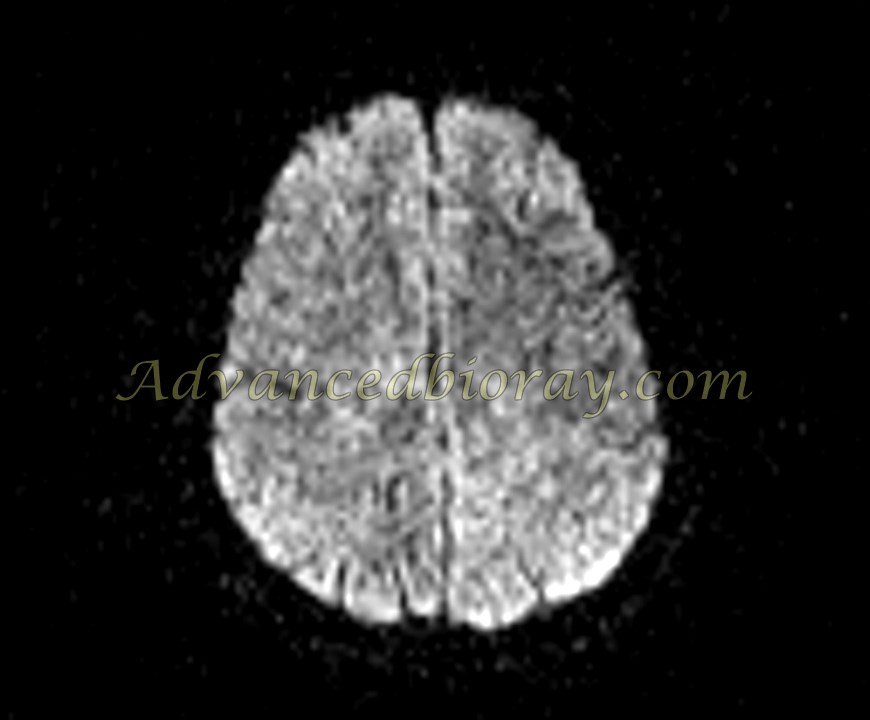
Case No 4
A 37-year-old woman presented with visual problems and blurred vision. One of the differential diagnoses for demyelinating diseases is Susac syndrome. This is a confirmed case of Susac syndrome (SS), a rare autoimmune microangiopathy that affects the brain, retina, and inner ear. The syndrome is characterized by a clinical triad of encephalopathy, branch retinal artery occlusions, and hearing loss. Brain MRI in this patient shows distinctive supratentorial white matter lesions, typically involving the corpus callosum with the characteristic “snowball sign.” The spinal cord survey is normal.